
NHS services are “failing to communicate properly” with people who are blind, deaf or have a disability, a patient watchdog has said.
Communication blunders range from deaf people being asked to book appointments over the telephone and blind people told to fill in paper forms.
Healthwatch England said two-thirds of NHS trusts are not giving people with additional communication needs equal access to care.
It said the NHS needs to act to make sure that no-one is excluded from access to healthcare, as it released new data showing that a number of NHS bodies are not meeting their legal obligation to provide accessible and understandable information to patients with disabilities and those who are deaf or blind.
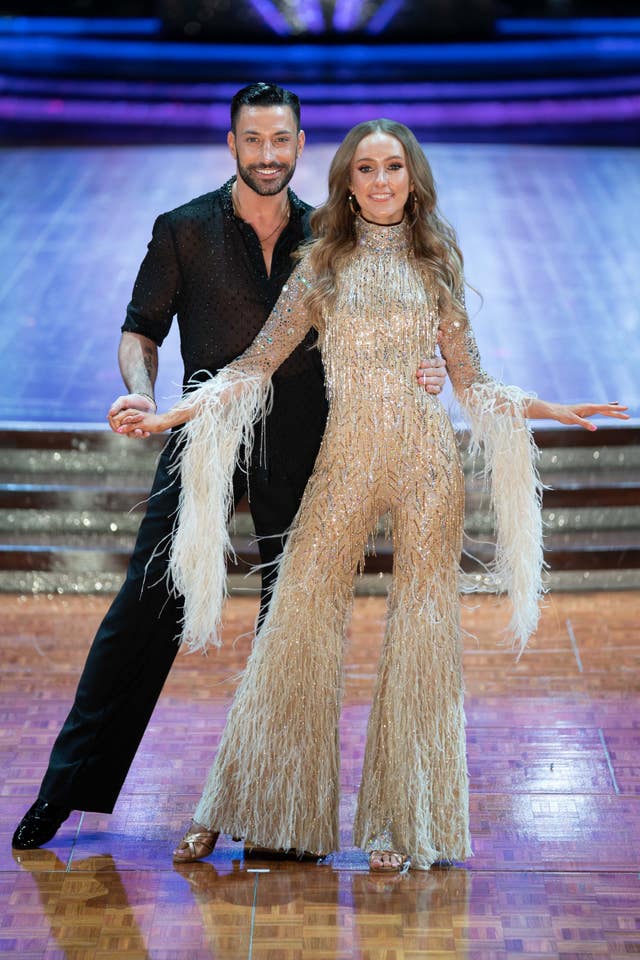
Strictly Come Dancing champion and EastEnders actor Rose Ayling-Ellis has previously spoken out about difficulties when accessing health services.
She told the BBC in January: “If I go to the doctor and there is no interpreter, it means I have to bring a family member with me.
“But I don’t want that, I want privacy.”
Healthwatch England set out to assess how NHS trusts were providing communication to patients after it saw a 141% surge in reports related to healthcare information during the first year of the pandemic compared to the same period before Covid-19 hit.
It also conducted a review of 6,200 people’s experiences between April 2019 and September 2021.
The information concluded that changes to services that took place during the pandemic were especially acute for people who are blind, deaf or have a learning disability.
Communication errors reported to Healthwatch England include a blind person given paper forms to order a white cane and deaf people being asked to book GP appointments over the phone.
Some deaf people reported that staff tried to communicate with them by shouting.
A number of people reported that services were unable or unwilling to provide them with support such as a GP provider refusing to use a sign language interpreter.
When provisions were not made, people felt as though they had to share private health information with family members who needed to accompany them to their appointments.

Healthwatch also warned that implementation of the Accessible Information Standard, a legal requirement created by NHS England in 2016 to ensure health and social care providers share and meet the information and communication needs of those who use their services, was “patchy”.
It found that only 35% of NHS trusts fully complied with the standard.
Of 139 organisations which responded to Freedom of Information requests, only just over half (53%) of trusts reported that they ask patients about their communication needs and what support they need when the patient first engages with services.
A quarter (26%) of services did not record a patient’s communication needs on their patient file or only did this some of the time.
And only 57% of trusts said staff routinely share a patient’s communication needs with other health and care services.
Healthwatch said some trusts admitted that low staff awareness of accessible communication, constrained resources and a lack of IT systems that would allow them to record patients’ communication needs.
Sir Robert Francis QC, chair of Healthwatch England said: “Our findings show clear evidence of a failure to protect the rights of our most vulnerable patients to accessible information and communication support through poor accountability across our health services.
“Health and care services are legally required to follow the Accessible Information Standard, yet currently there is no effective mechanism for holding them to account on how they put it into practice.
“People want clear, understandable information to enable them to make informed decisions about their health and care and get the most out of services.
“This research shows that health and care services must act to ensure no-one is excluded from access to healthcare because of their communication needs.”
Connor Scott-Gardner, who is blind, said a few minor changes and training for NHS staff would “make the world of difference” to help him use services.
The university student from Leeds, who requires healthcare information in an electronic format as well as in Braille, said: “I feel forgotten, ignored and not taken seriously.
“All I’m asking for is consistency, training on accessible information for staff – a few minor changes would make the world of difference to people like myself.
“I want to be able to take responsibility for myself, and good accessibility gives me the choice and freedom to do that. When it’s accessible, there’s nothing I can’t do.”
Healthwatch England released its findings as the NHS is reviewing the Accessible Information Standard and the British Sign Language Bill has reached the Committee stage of the legislative process.
The proposed legislation would give legal protection to the language in the UK.
Healthwatch and a coalition of charities including SignHealth, RNIB and Mencap have set out a series of recommendations to ensure accountability of NHS services to make sure they deliver accessible and understandable information to patients who are deaf, blind or disabled.
An spokesperson for the NHS in England said: “All NHS services have a legal duty to provide clear and appropriate methods of communication to ensure that patients, service users and carers understand everything they need to about their treatment and care.
“NHS England is currently reviewing the Accessible Information Standard, including how to better ensure that people’s communication needs are met.”


Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules here